About the R-NEET project
Why the focus on depression among African youth?
Youth depression is a global emergency.
Sub-Saharan African youth are especially vulnerable to depression:
- they are a fast-growing population living on a continent threatened by the climate emergency
- livelihood and humanitarian challenges
- mental illness stigma
- and limited mental health services
These combined challenges fuel risk for depression and jeopardise the potential economic and social dividends of a fast-growing population of African youth.


Why the focus on NEETs in SA and Nigeria?
Depression is strongly associated with being NEET.
- NEETs are caught up in a vicious cycle of limbo-like ‘waithood’,
- socioeconomic precarity,
- and psychological distress.
Studying the experience of NEETs focuses our work on one especially vulnerable population that is common across Africa (1 in 5 sub-Saharan African youth is NEET), but also diaspora communities elsewhere. NEET rates are elevated in SA and Nigeria, with at least 1 in 3 youth being NEET.
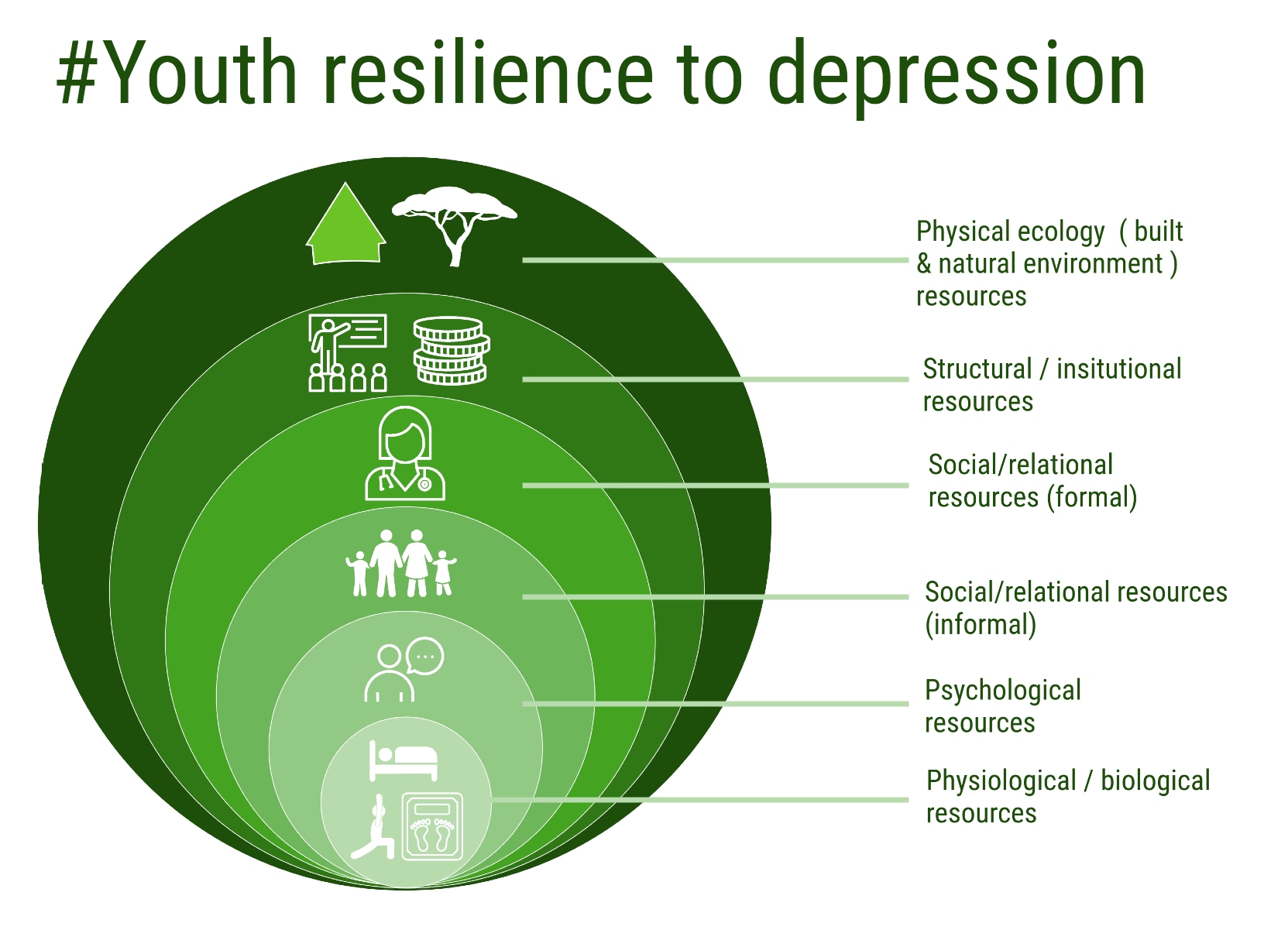
Why the focus on a multisystemic combination of resilience-enablers?
Resilience, or the capacity to respond adaptively to significant stress (like being NEET), is more than personal strength. Instead, significantly stressed youth who show resilience (e.g., no or minimal symptoms of depression) are supported by a contextually relevant combination of physical, psychological, social, economic, institutional, and environmental resources.
Currently, we do not know which precise multisystemic combination of risks and resources predicts depression trajectories among African youth who are NEET, or how situational and cultural context shape this combination at a point in time and over time. Discovery of this combination will advance Africa-centred accounts of resilience and further precision medicine and social interventions to prevent and manage depression.
Adapted from Ungar, M., & Theron, L. (2020). Resilience and mental health: How multisystemic processes contribute to positive outcomes. Lancet Psychiatry, 7(5), 441–448. https://doi.org/10.1016/S2215-